2022 FSA Podium and Poster Abstracts
S005: POTENTIAL CLINICAL UTILITY OF TIME-MULTIPLEXED SHARED VENTILATION
Jacob Q Yarinsky; Heiko Enderling, PhD, FSMB; Aaron R Muncey, MD; H. Lee Moffitt Cancer Center and Research Institute
Intro/Background: Hotspots of COVID-19 hospitalizations have caused ventilator shortages and require clinicians to decide which patients receive the mechanical ventilation they all need. One proposed technique to combat this is shared ventilation. It involves ventilating multiple patients with a single ventilator. While this technique has proven a ventilators ability to deliver pressures and tidal volumes to satisfy multiple patients, the technique does not account for patient-to-patient variability in ventilation need or pulmonary mechanics and include many severe risks.
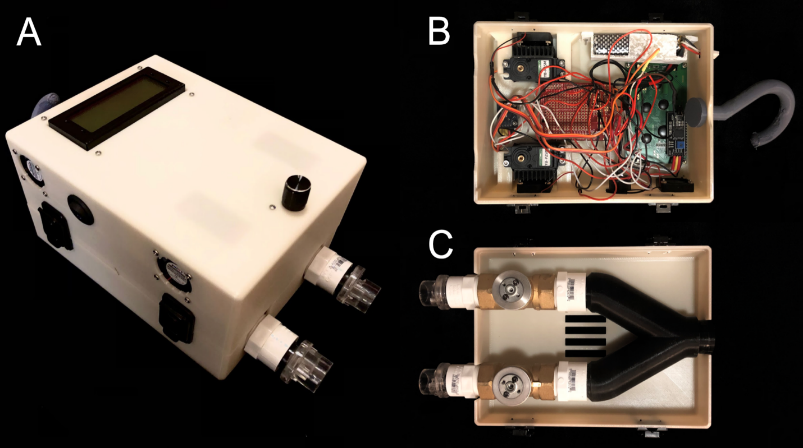
Methods: To address the technique’s lack of dynamic patient specific control, we developed a device that can ventilate multiple patients with independently controllable pressures. Unlike other co-ventilation devices, this device capitalizes on a ventilators ability to produce consistent pressure waveforms at respiratory rates double that of a single patient. The device uses electromechanically controlled valves to distribute and modulate the breaths in an alternating pattern to each patient. Theoretical and experimental analysis of temporally split co-ventilation was performed to determine clinical impact compared to simultaneous breath circuit configurations in test lungs.
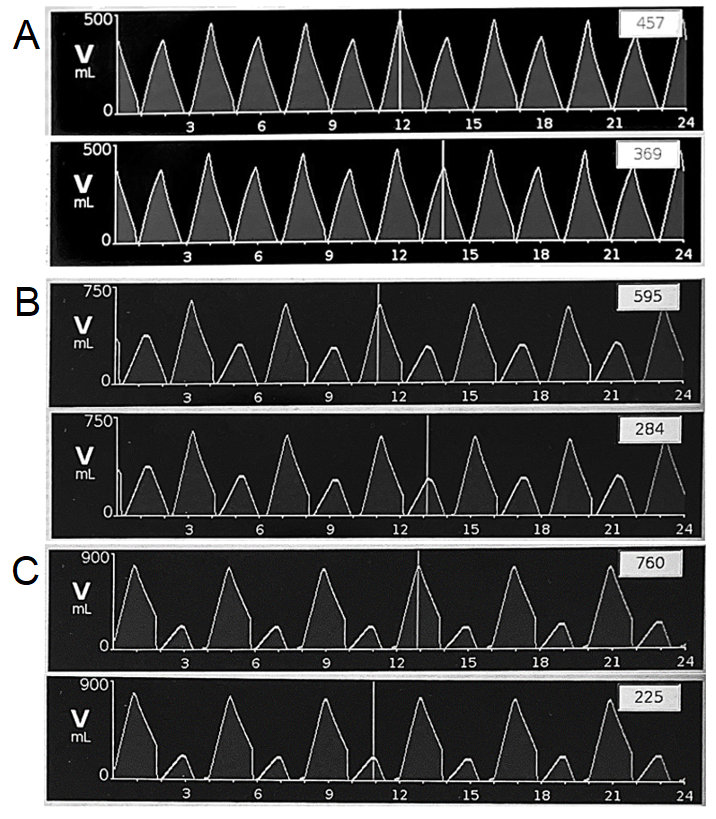
Results: The time-multiplexing approach was theoretically and experimentally successful in modulating the inspiratory pressure of the ventilator to each patient. It enabled monitoring of each patient's tidal volume to allow for clinical decision making for parameter adjustment. Compared to other co-ventilation circuits, occlusions and coughs with this device has minimal effect on the other patient. Dynamic aspects of pulmonary compliance caused by a progressing disease was able to be identified and accounted for with this device. The device was able to successfully ventilate test lungs with different pressure and tidal volumes. Tidal volumes of many different combinations, representing multiple patient combinations were also achieved.
Discussion: This device addresses many of the downfalls of the current, rudimentary, co-ventilation technique. It enables clinicians to remove the patient matching requirement and provide accurate patient specific pressures independent of the other patient. Being electromechanical, it also enables for dynamic control of pressure delivery. It also allows for clinicians to monitor individual patient tidal volumes and their evolving pulmonary mechanics. Further preclinical and clinical testing is needed for potential FDA approval, however potential clinical impact is clear. With this device available in the clinic, implementation of safe co-ventilation can be performed without hesitation.