2021 FSA Posters
P036: POSTOPERATIVE OPIOID SPARING AFTER TOTAL SHOULDER ARTHROPLASTY BY UNDILUTED EXPAREL SINGLE SHOT INTERSCALENE BLOCK
Enrico M Camporesi, MD1; Justin Christensen, MD1; Lauren Jindia, MD1; Suvikram Puri, MD1; Maha Balouch1; Georges Haidamous, MD2; Mark Frankle, MD2; 1TEAMHealth Anesthesia; 2University of South Florida
Introduction: Recent published studies have minimized the clinical effectiveness of Exparel. The purpose of this study was to prospectively compare the effects a single shot undiluted Exparel interscalene block, to Ropivacaine, supplemented with continuous catheter infusion, on postoperative opioid use following shoulder arthroplasty. This prospective, randomized study was pre-registered on the National Clinical Trials registry (NCT03739021).
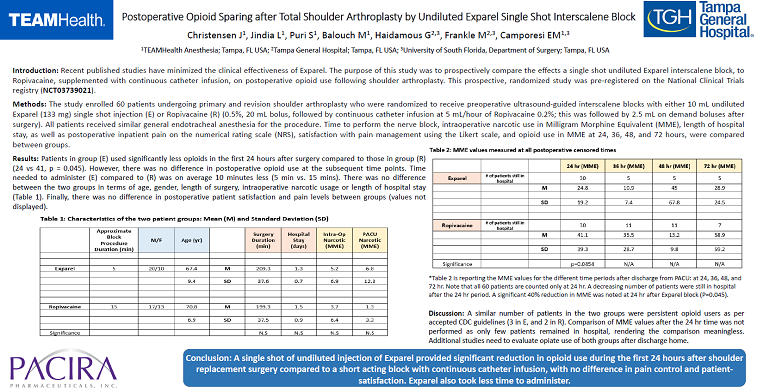
Methods: The study enrolled 60 patients undergoing primary and revision shoulder arthroplasty who were randomized to receive preoperative ultrasound-guided interscalene blocks with either 10 mL undiluted Exparel (133 mg) single shot injection (E) or Ropivacaine (R) (0.5%, 20 mL bolus, followed by continuous catheter infusion at 5 mL/hour of Ropivacaine 0.2%; this was followed by 2.5 mL on demand boluses after surgery). All patients received similar general endotracheal anesthesia for the procedure. Time to perform the nerve block, intraoperative narcotic use in Milligram Morphine Equivalent (MME), length of hospital stay, as well as postoperative inpatient pain on the numerical rating scale (NRS), satisfaction with pain management using the Likert scale, and opioid use in MME at 24, 36, 48, and 72 hours, were compared between groups.
Results: Patients in group (E) used significantly less opioids in the first 24 hours after surgery compared to those in group (R) (24 vs 41, p = 0.045). However, there was no difference in postoperative opioid use at the subsequent time points. Time needed to administer (E) compared to (R) was on average 10 minutes less (5 min vs. 15 mins). There was no difference between the two groups in terms of age, gender, length of surgery, intraoperative narcotic usage or length of hospital stay (Table 1). Finally, there was no difference in postoperative patient satisfaction and pain levels between groups (values not displayed).
Conclusion: A single shot of undiluted injection of Exparel provided significant reduction in opioid use during the first 24 hours after shoulder replacement surgery compared to a short acting block with continuous catheter infusion, with no difference in pain control and patient-satisfaction. Exparel also took less time to administer.
Table 2 is reporting the MME values for the different time periods after discharge from PACU: at 24, 36, 48, and 72 hr. Note that all 60 patients are counted only at 24 hr. A decreasing number of patients were still in hospital after the 24 hr period. A significant 40% reduction in MME was noted at 24 hr after Exparel block (P=0.045).

Discussion: A similar number of patients in the two groups were persistent opioid users as per accepted CDC guidelines (3 in E, and 2 in R). Comparison of MME values after the 24 hr time was not performed as only few patients remained in hospital, rendering the comparison meaningless. Additional studies need to evaluate opiate use of both groups after discharge home.
Supported in part by a grant from Pacira Biosciences, Inc.