2021 FSA Posters
P022: ACUTE TRANSIENT SIALADENITIS FOLLOWING ROBOTIC ASSISTED LAPAROSCOPIC CHOLECYSTECTOMY
Matthew Schepel, MD; Austin Smith, DO; Nicholas Nedeff, MD; Kendall Regional Medical Center
Introduction/Background: A 28-year-old female with no past medical or surgical history presented to the Emergency room for RUQ abdominal pain associated with nausea and vomiting. The patient was diagnosed with acute cholecystitis on CT imaging, admitted as an inpatient and consented for robotic assisted laparoscopic cholecystectomy.
Methods: Preoperatively, IV access with an 18G cannula was secured and the patient was premedicated with IV midazolam and transdermal scopolamine patch. In the operating room, standard monitoring equipment was connected and induction of anesthesia achieved with fentanyl, lidocaine, and propofol; succinylcholine was administered to facilitate oral endotracheal intubation and anesthesia maintained with oxygen and 2 percent sevoflurane. For intubation a Mac three blade was used for direct laryngoscopy. A grade one view of the cords was visualized, and no difficulties arose during the airway management. The endotracheal tube was fixed to the right side of the mouth via skin tape without any pressure to the cheeks. Cefazolin was administered prior to first incision. Dexamethasone, ondansetron, and ketorolac were administered in the perioperative period, and rocuronium was titrated throughout the case for muscle relaxation. At the conclusion of the procedure, muscle relaxation was reversed with neostigmine and glycopyrrolate, and the patient was extubated in the immediate postoperative period without complications. The immediate postoperative course was uneventful and the patient was admitted overnight for observation.
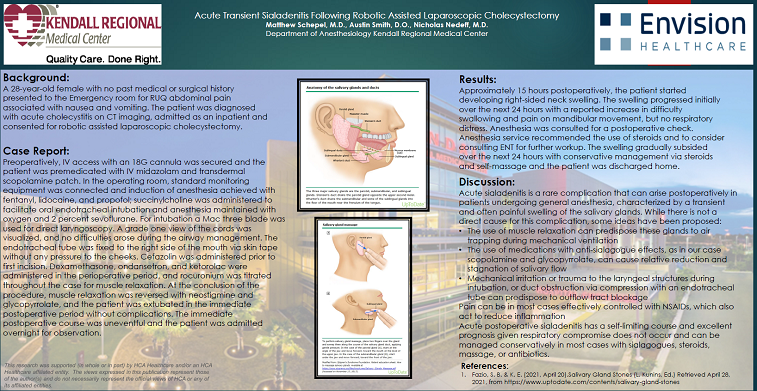
Results: Approximately 15 hours postoperatively, the patient started developing right-sided neck swelling. The swelling progressed initially over the next 24 hours with a reported increase in difficulty swallowing and pain on mandibular movement, but no respiratory distress. Anesthesia was consulted for a postoperative check. Anesthesia service recommended the use of steroids and to consider consulting ENT for further workup. The swelling gradually subsided over the next 24 hours with conservative management and the patient was discharged home.
Discussion/Conclusion: Acute sialadenitis is a rare complication that can arise postoperatively in patients undergoing general anesthesia, characterized by a transient and often-painful swelling of the salivary glands. While there is not a direct cause for this complication, some ideas have been proposed. The use of muscle relaxation can predispose these glands to air trapping during mechanical ventilation, as can the use of medications that dry up secretions, such as those used in reversal agents for muscle relaxation. Abdominal and gynecological cases are thought to be a risk factor to develop this because of the routine use of muscle relaxation. The use of pre and perioperative medication with an antisialogogue effect, in our case scopolamine and glycopyrrolate, can be an inciting predisposing factor for this complication’s development as a possible cause. Acute postoperative sialadenitis has a self-limiting course and excellent prognosis given respiratory compromise does not occur, and can be managed conservatively in most cases with sialogogues, steroids, massage, or antibiotics.