2021 FSA Posters
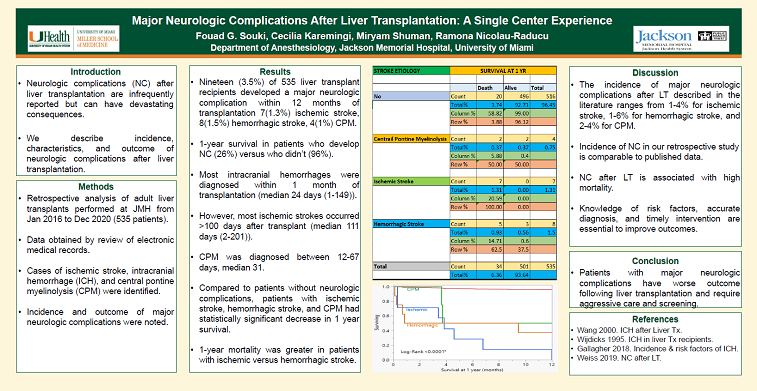
P016: INCIDENCE AND OUTCOME OF MAJOR NEUROLOGIC COMPLICATIONS AFTER LIVER TRANSPLANTATION: A RETROSPECTIVE SINGLE CENTER EXPERIENCE
Fouad G Souki1; Miryam Shuman2; Cecilia Karemingi2; Ramona Nicolau Raducu1; 1University of Miami; 2Jackson Memorial Hospital
Introduction: Neurologic complications after liver transplantation are infrequently reported but can have devastating consequences.
Methods: We performed a retrospective analysis of all liver transplants performed between January 2016 and December 2020 at University of Miami/Jackson Memorial Hospital using a prospectively maintained electronic database and query of the electronic medical record. Cases of ischemic stroke, intracranial hemorrhage, and central pontine myelinolysis (CPM) were identified. Characteristics and outcome of patients with major neurologic complications were analyzed.
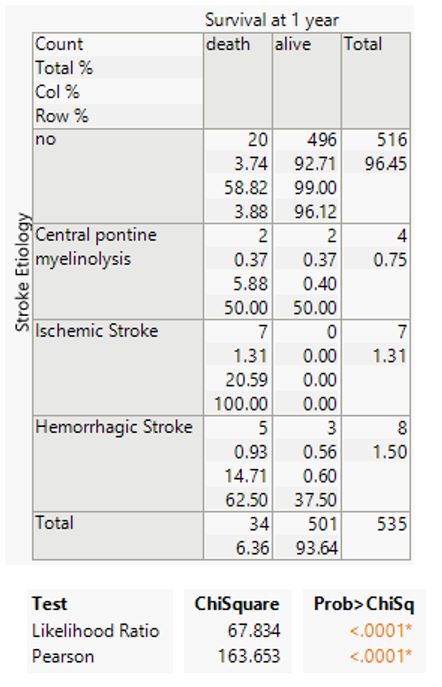
Results: Eighteen (3.4%) of 535 liver transplant recipients developed a major neurologic complication within 12 months of transplantation (7 ischemic stroke, 7 hemorrhagic stroke, 4 CPM). Most intracranial hemorrhages were diagnosed within 1 month of transplantation (median 24 days (1-149)). However, most ischemic strokes occurred >100 days after transplant (median 111 days (2-201)). CPM was diagnosed between 12-67 days, median 31. Compared to patients without neurologic complications, patients with ischemic stroke, hemorrhagic stroke, and CPM had statistically significant decrease in 1 year survival (0%, 38%, and 50% respectively)(Table 1, Figure 1). 1-year mortality was greater in patients with ischemic versus hemorrhagic stroke.
Conclusion: Patients with major neurologic complications have worse outcome following liver transplantation and require aggressive care and screening.

.JPG)