2020 FSA Posters
P085: EVALUATION AND TREATMENT OF POST-CIRCUMCISION BLEEDING IN AN INFANT
Sandra N Gonzalez, MD; Sonia D Mehta, MD; University of Florida
Introduction/Background: Circumcision is one of the most common surgical procedures in the pediatric population, with approximately 59% of male infants in the United States undergoing circumcision during the neonatal period. The rate of complications with circumcision is low, bleeding being the most common, with an estimated incidence of 1%. The following case illustrates the evaluation and treatment of post-circumcision bleeding.
Methods: Literature review, case report.
Results: A 9 month old male infant presents for elective circumcision for the treatment of penile adhesions. His past medical and family history are unremarkable. Circumcision is performed uneventfully under general anesthesia. Postoperatively, persistent bleeding is noticed from surgical site. Surgeon achieves partial hemostasis by applying silver nitrate and microfoam dressing. However, persistent bleeding is noticed on follow up appointment the next day. Patient is admitted for surgical revision. During pre-anesthesia assessment, multiple bruises in different stages of healing are noticed, as well as hematomas in previous venipuncture sites. Mask induction is conducted, and IV access obtained. Coagulation panel, CBC, and type and crossmatch for PRBCs are sent, revealing hemoglobin 6.5gr/dL and PTT 87, with normal PT/INR, platelet count, and fibrinogen levels. Surgical findings were generalized bleeding without identifiable single vessel as the source of bleeding. Transfusion of PRBCs and FFP was performed for correction of anemia and coagulopathy. Hematology evaluation confirms diagnosis of hemophilia A, with factor VIII activity of <2%, normalization of PTT with 1:1 mixing test, and absence of factor inhibitor. Further genetic testing confirms intron 22 inversion, and patient is enrolled in factor replacement program.
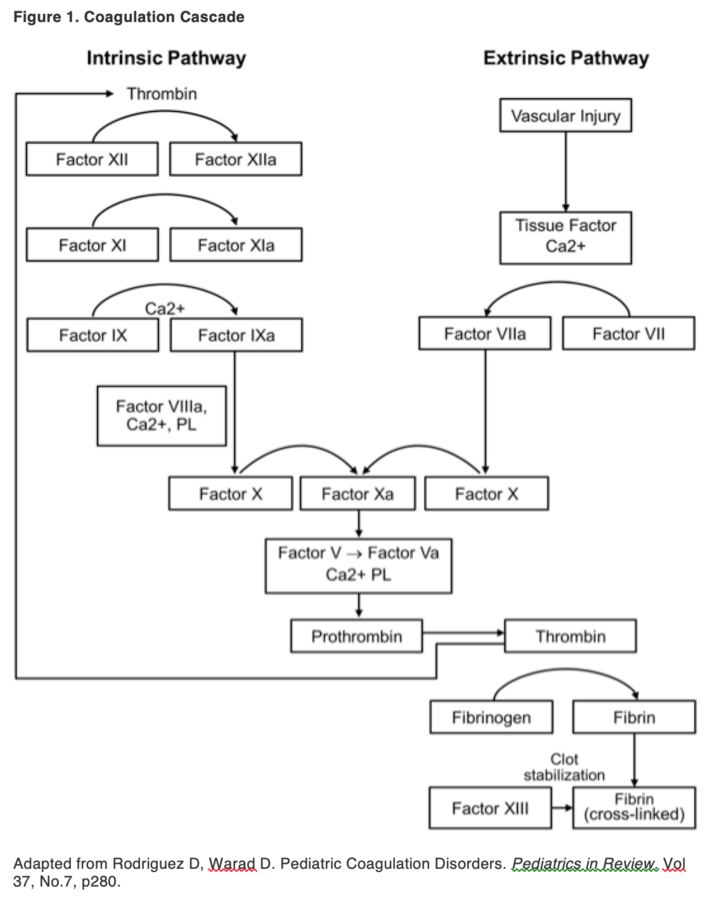
Discussion: Bleeding is the most common complication of circumcision, and while most cases will be successfully treated with surgical hemostasis, coagulation disorders must be considered in differential diagnosis if bleeding is persistent (Table 1, Figure 1). Absence of family history of coagulopathy doesn’t exclude diagnosis of hemophilia, as 30% of hemophilia A cases are due to de novo mutations, and in infants, surgical procedures can be the setting in which it is identified. 81% of infants with hemophilia A present bleeding in the first 2 years of life, with mucocutaneous bleeding, circumcision, and intracranial hemorrhage being the most common presentations, in contrast to the presence of hemarthrosis in older patients. Findings on physical exam can be confused with non-accidental trauma, which also must be considered. Children who have known diagnosis of hemophilia and require circumcision can be treated with the Izmir protocol, which includes the use of tranexamic acid preoperatively, factor replacement before and after circumcision, and intraoperative use of fibrin glue, with good results.
Conclusion: The presence of persistent post-surgical bleeding can be the presentation of coagulopathy in infants, and a thorough evaluation is required to adequately diagnose and treat the patient, counsel the parents and the family, and decrease the risk of future complications.
References:
1. Krill A, Palmer J. Complications of circumcision. ScientificWorldJournal. 2011; 11: 2458–2468
2. Complications of Hemophilia in babies: a report from the CDC Universal Data Collection System. R. Kulkarni, R.J. Presley. Haemophilia (2017), 23, 207-214.
.png)
