2020 FSA Posters
P013: MULTICENTER EVALUATION OF OPIOID USE AFTER AN INITIATIVE TO INCREASE MULTIMODAL ANALGESICS
Adam Fier, DO; Michael Sanchez, PharmD, BCCCP; Jay Pauly, PharmD, BCPS; Health First Holmes Regional Medical Center
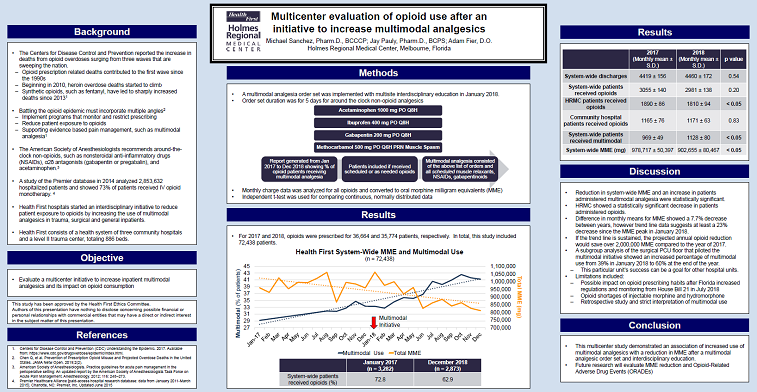
Introduction/Background: The Centers for Disease Control and Prevention described the latest wave of the opioid epidemic surging due to synthetic opioids, such as fentanyl. Florida has responded to the opioid crisis with increased regulation and prescription drug monitoring. Supporting evidence-based pain management, like multimodal analgesics, is a tactic to combat the opioid epidemic from the inpatient setting. The purpose of this study is to evaluate opioid consumption after an initiative to increase inpatient multimodal analgesics.
Methods: This retrospective evaluation was conducted in a health system of three community hospitals and a level II trauma center. A multimodal analgesic order set was implemented with provider education throughout this health system in January 2018. A report generated from the electronic medical record determined the percentage of patients who received non-opioid analgesic adjuvants when prescribed opioids. Data was analyzed before and after implementation from January 2017 through December 2018. Non-opioid analgesics included scheduled orders for acetaminophen, nonsteroidal anti-inflammatory drugs, gabapentinoids, or muscle relaxants. Opioid consumption was determined through hospital charges and converted to oral morphine milligram equivalents (MME). The primary endpoint was to evaluate the monthly mean consumption of opioids in MME for the health system. Secondary endpoints consisted of monthly mean multimodal use, patients administered opioids and hospital discharges.
Results: A total of 72,438 patients were included in the study, with 36,664 patients in the year 2017 and 35,774 patients in the year 2018. Health system-wide hospital monthly discharges did not differ between years (4,419 ± 156 vs. 4,460 ± 172; p=0.54). The health system-wide average of patients administered opioids did not differ (3,055 ± 140 vs. 2,981 ± 138; p=0.2), however the level II trauma center had a statistically significant reduction in patients administered opioids (1,891 ± 86 vs. 1,810 ± 94; p<0.05). Non-opioid analgesic use had a statistically significant increase throughout the health system (969 ± 49 vs. 1,128 ± 80; p<0.05). The health system demonstrated a statistically significant reduction in MME between years (978,717 ± 50,397 vs 902,655 ± 80,467; p<0.05).
Discussion/Conclusion: The trend line data showed a 23% MME decrease at the end of the study when compared to the peak MME in January 2018. If the final month of this study’s MME were sustained, the projected annual opioid reduction would save over 2,000,000 MME compared to the year of 2017. Limitations of this study were its retrospective nature and the impact on opioid prescribing from Florida’s House Bill 21 in July 2018. Although, trend lines showed a reduction in MME that correlated with the multimodal initiative starting in January 2018. Opioid shortages of injectable morphine and hydromorphone may have also affected the study, however opioid dispensing was shifted to alternate dosage strengths instead of patients going without injectable opioids.
This multicenter study demonstrated an increased use of non-opioid analgesics with a reduction in MME after implementing a multimodal analgesic order set. Further research may evaluate MME reduction with opioid-related adverse drug events (ORADEs), pain scores and patient satisfaction.