2018 FSA Posters
P054: ONGOING ASSESSMENT OF A SELF-STUDY, SELF-DEBRIEFING SIMULATOR FOR CENTRAL VENOUS ACCESS: PRELIMINARY RESULTS
Samsun Lampotang, PhD, Edward McGough, MD, FCCP, Joshua Sappenfield, MD, Nikolaus Gravenstein, MD, Lou Ann Cooper, PhD, Dave Lizdas, BMES, Anthony Destephens, MSME, Andrew Gifford, BS, Desmond Zeng, MS; University of Florida Department of Anesthesiology
Background: Central venous catheter (CVC) insertion is a common invasive procedure performed in the ICU.1 CVCs are typically inserted percutaneously through large veins such as the subclavian and jugular veins. Common complications are pneumothorax (PTX) and arterial puncture. Proper training should help lower complication rates. Because faculty and trainee time are valuable, we are investigating the efficacy of the UF Mixed Reality Central Venous Access (CVA) Simulator for training our anesthesiology, internal medicine, emergency medicine residents, nurse practitioners, and physician assistants. This simulator has an integrated tutor (IT) that includes 3-D visualization of the virtual anatomy and tracked tools, cognitive aids (e.g. needle alignment with ultrasound, US insonation plane), video instruction and other self-study tools (e.g. built in quiz questions) and self-debriefing. We hypothesize that this simulator can efficaciously deliver a self-study/self-debriefing curriculum that promotes acquisition of procedural skills.
Methods: With IRB approval after power analysis/sample size calculation, 54 UF trainees will be assessed on their ability to obtain central venous access via both internal jugular (IJ) and subclavian (SC) approaches. Participants are randomly assigned to either instruction via the UF CVA simulator with integrated tutor (IT) or the simulator with scripted instruction and feedback from a UF Department of Anesthesiology faculty member (HUM). After consent, we assessed baseline performance for US-guided IJ access and landmark-based infraclavicular SC access. Participants were then taught both methods of obtaining central venous access by either the integrated tutor (IT) or by a human instructor (HUM). After instruction, participants were evaluated on 6 trials per approach, 3 normal veins and 3 small veins. US-guided short axis and long axis techniques were required for IJ. Successful access was defined as obtaining venous access within 3 attempts without PTX or arterial puncture.
Results: To date, 48 participants of our target of 54 have completed the study (IT=25; HUM= 23). We report the results of the non-inferiority analysis for the proportion difference assuming a noninferiority margin of 15%. (H0: IT-HUM £ -.15 vs. Ha: IT-HUM > -15). All trials were normal anatomical difficulty. :
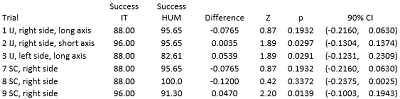
Since the noninferiority margin, -.15, does not fall within the confidence interval, we conclude that IT is non-inferior to human instruction for trials 2, 3, and 9.
Conclusions: Preliminary results suggest that the IT group is non-inferior to the HUM group in trials 3 and 9. As the study progresses, we expect that the UF Mixed Reality Central Venous Access Simulator will continue to produce training outcomes that are non-inferior to traditional faculty-led instruction, in selected specific skills and techniques.
