2018 FSA Posters
P047: ANALGESIA POST ABDOMINAL SURGERY: A SEQUENTIAL CASE SERIES COMPARING INTRAVENOUS PAIN MANAGEMENT VS. CONTINUOUS THORACIC EPIDURAL PAIN MANAGEMENT
S Puri, MD1, M Copeland, BS2, G Enten, BS1, D Mangar, MD1, E Camporesi, MD1; 1TEAMHealth Anesthesia, 2University of South Florida
Introduction/Background: Few reports have evaluated continuous thoracic epidural analgesia effects on common abdominal surgeries as compared to more traditional intravenous pain control methods. The introduction of new pain group at Tampa General Hospital and application of new guidelines for the year 2017 affords the opportunity for a sequential case series analysis of these two methods of pain management.
Methods: A sequential case-series on patients undergoing laparoscopic or robot assisted abdominal surgery was performed. Patients were recruited upon request of surgeons at Tampa General Hospital, using the same resident support team. Data were obtained from retrospective chart review following IRB approval from the University of South Florida and evaluated for the effects of intravenous analgesia compared to continuous bupivicaine T10 epidural analgesia. Intravenous group data were collected from January 2015 to December 2016; Epidural group data were collected from January 2017 to July 2017. Primary outcomes were intraoperative, 24 hour, and post-24 hour opioid use in morphine milligram equivalents (MME). Length of hospital stay and VAS pain scores were also collected. The control group had 30 participants (n=30) and the surgeries included 21 laparoscopic bowel resections, 4 of which were robot assisted, 3 bowel stoma creation, revision or reversals, 2 exploratory laparotomies with lysis of adhesions, 3 rectoplexies, and 1 cholecystectomy. The treatment group had 29 participants (n=29) and the surgeries included 20 laparoscopic bowel resections, 4 bowel stoma creation, revision or reversals, 1 fistula takedown, and 4 rectoplexies.
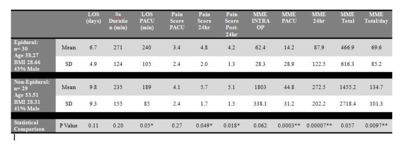
Results: Data were analyzed using a non-paired two-tailed t-test, significance was determined at a p-value < 0.05. Groups were comparable in age, gender, BMI, and surgeries performed. When compared to the patient series from January 2015 to Dec 2016, patients from Jan 2017 onward who received epidural reported significantly lower pain scores in the first 24 hours after surgery (p < 0.05) and for the remainder of their hospital stay (p < 0.05). Additionally, a significant decrease in narcotic use as measured by MME was noted in the PACU (p < 0.001), the first 24 hours after surgery (p < 0.001), and aggregate use per day (p < 0.01). While reduction in aggregate total use was not statistically significant a clinically significant reduction was noted from 1455.2 MME to 466.9 MME. A decrease in length of stay was also noted from 9.8 to 6. 7 days.
Discussion/Conclusions: Our study indicates that for patients undergoing common major abdominal surgical procedures, continuous thoracic epidural analgesia is a viable alternative to intravenous pain control. Further, it significantly reduced, pain scores as-well-as average MME use for the first 24 hours after surgery and resulted in quicker discharge time on average of 3 days.. More refined comparisons can be made by conducting a precise prospective study with a more structured protocol in place.