2017 FSA Posters
P036: MINI-AORTIC VALVE REPLACEMENT: A STITCH IN TIME
Oscar A A Alam Mendez, MD, Caryl Bailey, MD, Adriane Warrick, MD; University of Florida Jacksonville
Background: Aortic valve disease is the most common valvular heart disease in developed countries. Its incidence is 2-4% in people aged more than 65-85 respectively. Conventional aortic valve replacement (AVR) with a full sternotomy (FS) using cardiopulmonary bypass (CPB) is the gold standard technique. A minimally invasive aortic valve replacement (MIAVR) refers to AVR, which involves a small chest incision as opposed to the FS. The two most common approaches are: ministernotomy (MS) and the right anterior minithoracotomy (RT). While the RT has shown superior outcomes to the MS, patients must meet specific imaging and clinical criteria for the RT approach. Other options are the right parasternal approach (requiring resection of the costal cartilages) and the transverse sternotomy. RT involves a 5-7 cm transverse incision at the 2nd intercostal space.
CPB cannulations sites can somewhat vary for MIAVR. It can be done through the femoral artery and vein or direct aortic cannulation with a flexible cannula. Fluoroscopy and transesophageal echocardiography are often used to aid cannula placement.
Specific anesthetic considerations related to MIAVR include lung isolation techniques, possible requirement for transvenous pacing, and placement transcutaneous defibrillator pads .
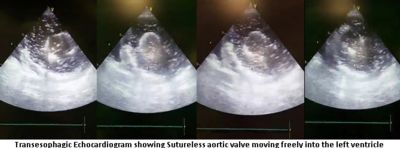
Case description: A 35 year old male with aortic regurgitation secondary to infectious endocarditis. He was to undergo MIAVR via RT approach. After induction, a 39 F double lumen endotracheal tube was placed. Central intravenous access was obtained at the right internal jugular vein. CPB cannulas were placed via the right common iliac artery and superior vena cava through right femoral vein. A sutureless Perceval valve was placed which initially appeared to be in good position, however, while separating from CPB, the valve became dislodged and fell into the left ventricle. This was noted immediately by TEE examination. After return to CPB, the valve was successfully retrieved and the patient received a mechanical AVR. TEE examination showed proper valve position and function. The patient was successfully weaned from CPB and transported to the ICU. His postoperative course was complicated by right hemothorax requiring surgical evacuation on post-op day 5. He was discharged to home on day 10 post MIAVR.
Discussion: Sutureless aortic valves are held in place by the outward force of its circular frame against the aortic valve annulus. The Perceval valve is used for conventional surgery since FDA approval in January 2016. It facilitates a minimally invasive approach due to easier placement technique and shorter time on CPB. The failure of the Perceval valve in this case was likely due to the lack of aortic annular calcification which resulted in the valve migration. This concept is similar to patients who undergo transcatheter aortic valve replacement (TAVR). As newer, safer, and less invasive approaches to cardiac surgery emerge, it is important to become familiar with the evolving equipment and products and be able to recognize complications and shortcomings of these newer procedures. Currently the two commercially available sutureless valves are the self-expanding Perceval S and the rapid-deployment Intuity elite. Of note, postoperative conduction disorders are more commonly encountered after sutureless AVRs.